Γιώργος Γεωργάτος MCPS BSc Physiotherapy, MSc, FCP. Ashford & St Peters NHS trust
===============
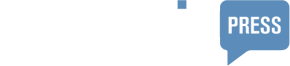
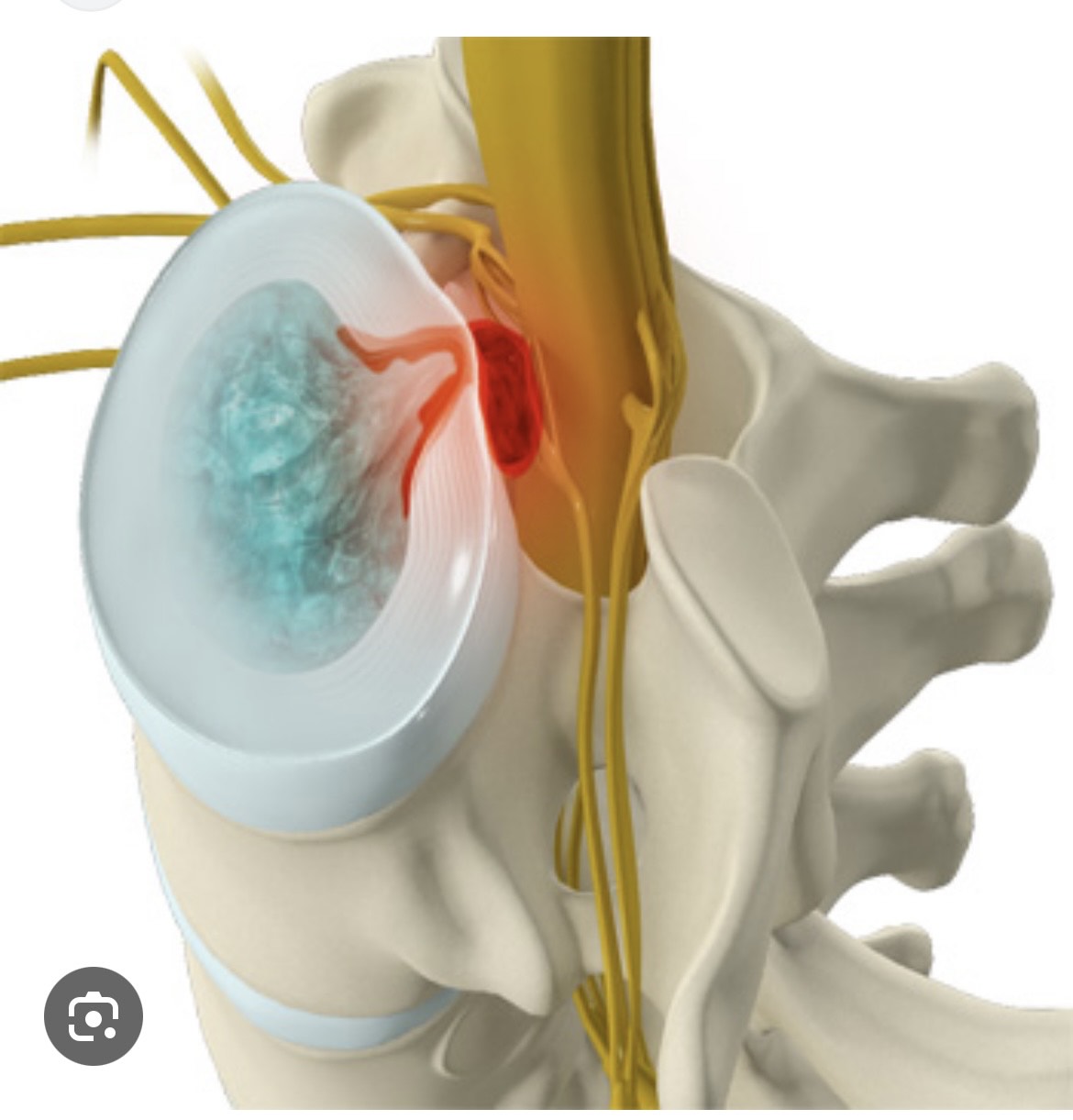
Cauda Equina Syndrome (CES) is a serious condition that occurs when the bundle of nerves at the lower end of the spinal cord (the cauda equina) is compressed.
This can lead to severe neurological damage if not treated promptly, affecting mobility, sensation, and even bladder or bowel function. Early detection and treatment are essential to prevent permanent disability. In remote areas, such as islands, managing Cauda Equina Syndrome can be challenging, particularly when access to medical facilities and specialists may be limited. Here’s how physiotherapy plays a critical role and what the challenges may look like in such settings:
Importance of Physiotherapy for Cauda Equina Syndrome: 1. Restoration of Function: After surgical intervention to relieve nerve compression, physiotherapy is essential for regaining strength, improving mobility, and enhancing balance. 2. Bladder and Bowel Control: Physiotherapists work with patients to manage pelvic floor strength, which can improve bladder and bowel function affected by CES. 3. Pain Management: Customized exercises and manual therapy help reduce pain, restore movement, and prevent secondary issues like muscle atrophy or joint stiffness. 4. Psychological Support: Living with the symptoms of CES can be distressing, especially in isolated areas. Physiotherapy can support mental well-being through movement therapies and coping strategies. 5. Prevention of Complications: Long periods of immobility can lead to additional problems, such as bedsores and infections.
Physiotherapists help patients stay mobile and avoid these issues. Challenges in Remote Places (like Islands): 1. Limited Access to Specialists: Remote islands often have fewer medical professionals, particularly those with specialized knowledge of CES. This can delay the start of physiotherapy, impacting recovery. 2. Rehabilitation Equipment and Facilities: Physiotherapy for CES may require specialized equipment for strengthening and mobility training, which might not be available in rural or island settings. 3. Telehealth and Remote Care: In the absence of local specialists, telehealth can play a significant role in providing remote guidance for exercises and rehabilitation protocols. However, limited internet connectivity or infrastructure could hinder this. 4. Travel Barriers: For ongoing physiotherapy, patients might have to travel long distances or between islands, which is both time-consuming and physically challenging for someone with CES-related disabilities. 5. Lack of Immediate Emergency Care: In cases where CES is suspected, immediate medical attention is crucial to prevent irreversible damage. In remote areas, timely surgery or intervention can be delayed, leading to worse outcomes. In these situations, physiotherapy must be adaptive, often relying on local resources and creative solutions to provide care. Training local healthcare workers or caretakers in basic rehabilitation exercises could be essential to improving the quality of life for patients in such areas.
Georgios Georgatos MCPS BSc Physiotherapy, MSc, FCP. Ashford & St Peters NHS trust